I Don’t Take Insurance. Do I Still Need to Write Treatment Plans and Progress Notes?
Yes! Documentation has always been a standard in our profession so it’s required. And here are other good reasons why.
- Even if you do not take insurance, if you see a client who has out-of-network benefits and uses a PPO, you can still be audited. This means you still have to justify medical necessity or risk claw backs. This has been happening more in recent years.
- Your records could be subpoenaed. Not only do you want to make sure they are HIPAA compliant for the protection of you and your client, it’s easier to have your notes written when they are fresh than to have to recreate the session when they are stale.
- You may have a client who goes out on Workman’s Comp or requests Disability. These entities can request your records and because the client wants the benefits, they sign the release.
- If the client is ever a danger to him/herself or others, you need to document your assessments and what you did in response. This needs to be done the day of the assessment, not after the problem occurred. This information could be called into question so you want it documented correctly.
- If a client sues, you need to have records to protect yourself. These records include all kinds of non-clinical information, including the actual start and stop time of the session and the date of the next session.
- Case and Collateral Contact Notes prove that you’ve communicated with other providers and gotten consultation on challenging cases. This could be important if you are ever sued by a disgruntled client or family or if you are trying to justify continued treatment with an insurance company.
- Discharge Summaries are important because if you do not formally discharge a client and something happens. In this case, the client might still be considered in your care and you can accused of or sued for negligence.
These are the “negative” or the cover-your-butt reasons to maintain good documentation.
Remember — IF IT’S NOT DOCUMENTED IT DIDN’T HAPPEN.
On the positive side, writing weekly notes can help you:
Stay focused on treatment goals, reflect on the session and discover something important for the next session. On a personal note, half my practice is private pay and I write progress notes for them as well as those on insurance. It doesn’t take long to write a session note and I like being able to reflect on what we did together, sometimes using any insights I gain during this review time for the next session.
Once you find a program or format you like, writing a progress note should take no longer than five minutes; seven minutes if the session is complicated. I like to write them after each session or at the end of the day so when I leave the office, I’m DONE for the day and don’t have hours of paperwork waiting for me at the end of the week. To write treatment plans is more complex so will take longer but 1) they only have to be done yearly in private practice and 2) writing the subsequent plan goes much faster.
A Diagnostic Summary is done after the first few sessions. You can’t always get all the information you might want but you need to develop a diagnostic formulation and decide on a diagnosis with the information you have. This way, you can write the treatment plan, decide on a diagnosis and bill the insurance company in a timely way. If you learn more later in the course of treatment, the diagnosis can always change, which would be reflected in your progress note. If this happens, you would ideally revise your treatment plan.
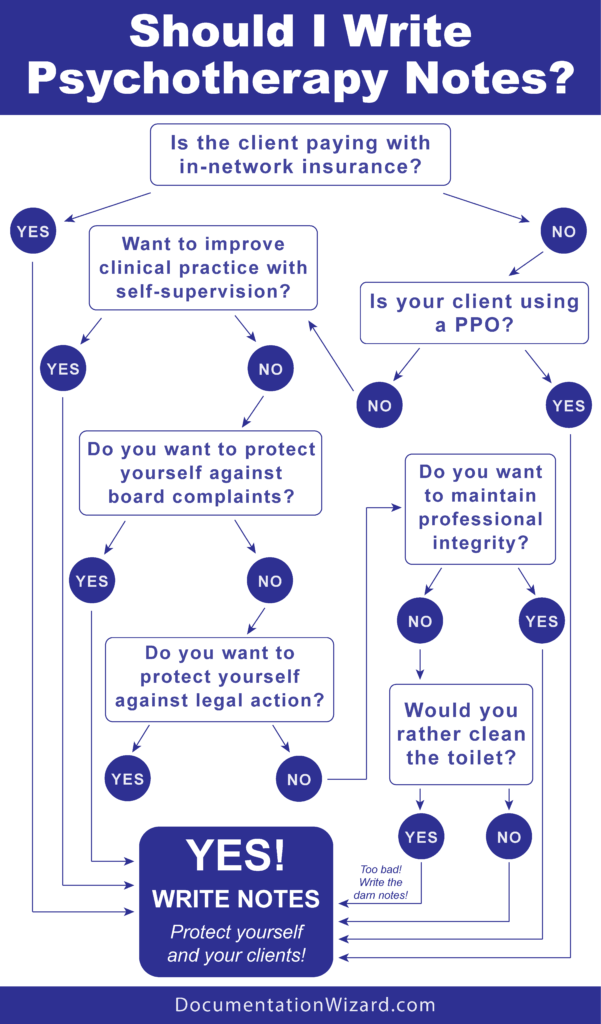
Still not sure if you should always write therapy notes? This flow chart can help you decide.
Documenting your work does take time and after a long day it’s not a welcome task but it could save you a lot of heartache — and contribute to your clinical work. You can become a Documentation Wizard through on my online workshop, Misery or Mastery: Documenting Medical Necessity for Psychotherapists. It guides you through the process of writing treatment plans, session notes, and the other essential clinical documents.