Are Discharge Summaries Mandatory?
Do you need to write a discharge summary as a mental health provider?
Yes and no.
Confusing? Definitely. That’s because the standards are not consistent from one insurance company to the next.
Here’s what I can tell you:
Discharge Summaries for Medicaid
Medicaid requires discharge summaries for mental health, particularly if the person is in inpatient. If you do not have one when audited, you will be out of compliance and likely incur a recoupment. For more information on their requirements for documentation, take a look at this pdf: https://www.cms.gov/Medicare-Medicaid-Coordination/Fraud-Prevention/Medicaid-Integrity-Education/Downloads/docmatters-casestudy-guide.pdf
Discharge Summaries for Medicare
After all the reading I’ve done, it appears that Medicare does not require discharge summaries. That doesn’t mean you shouldn’t do it. Keep reading for why writing a discharge summary, even if it isn’t required, could save you a lot of money and even your professional license.
Discharge Summaries for Commercial Insurance Companies
Documenting discharge for private insurance is up to the insurance company. Be proactive and call them to find out. But if they don’t require it, should you write one?
WHY WRITE A DISCHARGE SUMMARY?
Use best practice! Even though discharge summaries are not required by all companies, I highly recommended writing them even if you do not take insurance and only accept private pay clients. They are useful for the client and can protect you from legal action.
There are all kinds of issues that could lead to legal involvement. A client gets arrested, attempts or completes suicide, stops coming after you file a 51A, or gets embroiled in a nasty custody battle, to name a few.
Perhaps you have not seen the client for 3 months or even a year but if asked, the client or a family member refers to you as the therapist. Perhaps a distraught parent sues you for not protecting their teenage child from suicide even though the teenager stopped showing up for sessions. Or a former client gets arrested and the probation officer asks if they have a therapist and you’re named. Or your client fires you after you file a 51A.
If there is no discharge summary, you can be legally considered the therapist even if you have not seen the client for over a year.
When Should a Client be Discharged?
There is no hard and fast rule governing this practice. The decision is up to the individual therapist’s tolerance for risk. Here are some guidelines.
- If termination has been discussed and planned, write the discharge summary within a week after the last session.
- If the client has not shown or communicated for 2 weeks, write it then.
- Be proactive. Have a clause in your office policies about the number of no-shows and cancellations that will trigger termination.
OK, I get it. Write a discharge summary! But what do I write?
DISCHARGE SUMMARY REQUIREMENTS
- A review of the mental health treatment
- Reason for discharge
- Date of discharge
- Condition at discharge
- Response to psychotropic medications
- Collaterals notified
- Recommendations for aftercare
Protect yourself by always writing a discharge summary.
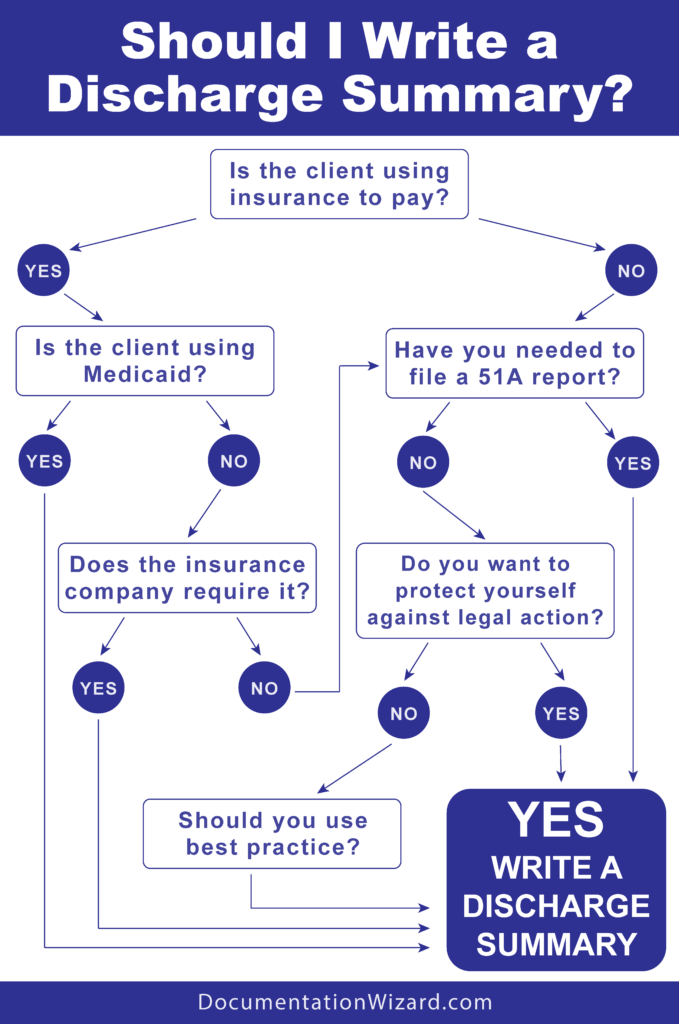
Here’s a helpful flow chart you can use to determine if you should write a discharge summary.
Need more guidance on how to write effective documentation? This is the kind of information I provide in my workshop on clinical documentation so you can protect your income, pass audits, maintain professional integrity, reduce your anxiety, and even learn to enjoy writing therapy notes.
Want a template for discharge summaries? Documentation Wizard provides templates for all clinical documentation needs that cue you to include everything needed so you can protect yourself legally and financially.